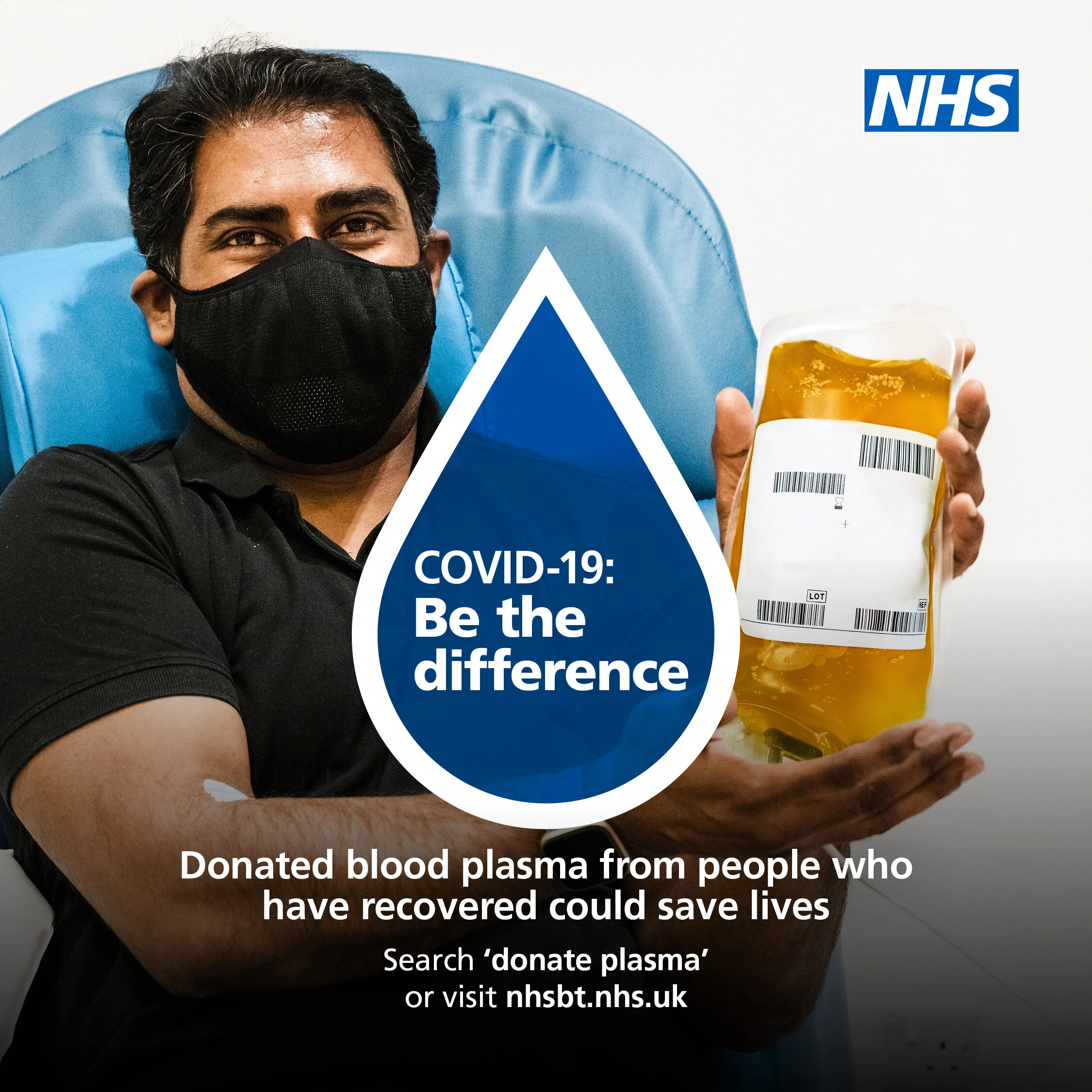
Renewed call for blood plasma donors
In the search for Covid-19 treatments, convalescent plasma trials continue to answer key questions for the most vulnerable patients.
Source: NHS Blood and Transplant
SPONSORED CONTENT
In the early stages of the pandemic, investigations began to establish whether the blood plasma from people who have recovered from Covid-19 may help alleviate the symptoms in the most gravely ill patients with the novel coronavirus. It is a treatment - known as convalescent plasma - that has been used to treat outbreaks of flu for over a century, including, more recently, Ebola. However, its efficacy has yet to be fully understood. Today, following two UK clinical trials and emerging global evidence, the picture is becoming clearer.
How does convalescent plasma work?
When infected with a virus, our immune systems recognise the invading pathogen and produce specific antibodies to inhibit it. This prevents the virus from entering cells and thereby spreading around the host’s body. Following recovery, these antibodies stay in the blood plasma - the straw-coloured liquid part of the blood. In convalescent plasma treatment, the antibody-rich blood plasma of a recovered patient is transfused into that of a sick patient, giving their immune system a helping hand. Meanwhile, the antibodies of the donor are quickly replenished.
Does it help treat Covid-19 patients?
In short, we don’t know yet. The Clinical Trials Unit at NHS Blood and Transplant (NHSBT) helped to deliver two separate trials, Recovery and REMAP-CAP. The former looked into the efficacy of convalescent plasma on moderately ill patients, while REMAP-CAP focused on those requiring organ support in ICU. Together, Recovery and REMAP-CAP provided the world’s largest randomised clinical trial on convalescent plasma.
Earlier this month, both trials reported interim results. On January 11, REMAP-CAP announced that results showed a 2.2 per cent probability that convalescent plasma was beneficial for the severely ill. While, the Recovery trial reported that its interim results did not show evidence that plasma has an overall benefit on patient outcomes in moderately ill people.
Both trials continue to analyse whether plasma could benefit subgroups of patients, such as those with naturally low antibody levels.
What next for blood plasma donors?
While both trials are in the data analysis phase, following discussions with the Department of Health and Social Care, NHSBT is continuing to collect plasma. This followed emerging evidence from Argentina that treatment with convalescent plasma can be effective if administered much earlier on in the course of the disease. The randomised controlled study, published in the New England Journal of Medicine, found that use within 72 hours of symptom onset, before hospital admission, reduced the occurrence of severe Covid by 50 per cent. A similar UK trial is being discussed.
Chief Medical Officer for NHSBT, Dr Gail Miflin, said: “The whole world is now focusing on early treatment, before organ damage and hospitalisation. Antibodies stop the virus, they don’t treat the damage it does.” [Commenting on the study] “This could particularly help the most vulnerable people, such as the elderly or those with weakened immune systems who do not respond well to vaccines. This includes more than a million people with blood cancers, organ transplants, chronic diseases and more.
“Given the ongoing trials and ongoing analysis, NHSBT, the DHSC [Department for Health and Social Care] and the Therapeutics Taskforce have agreed to keep collecting stocks of convalescent plasma. To be ready for the future, the time to collect is now.”
If you have tested positive for Covid-19 in the past or had symptoms, you can volunteer to donate plasma here.